How to recognize the signs and symptoms of CTX
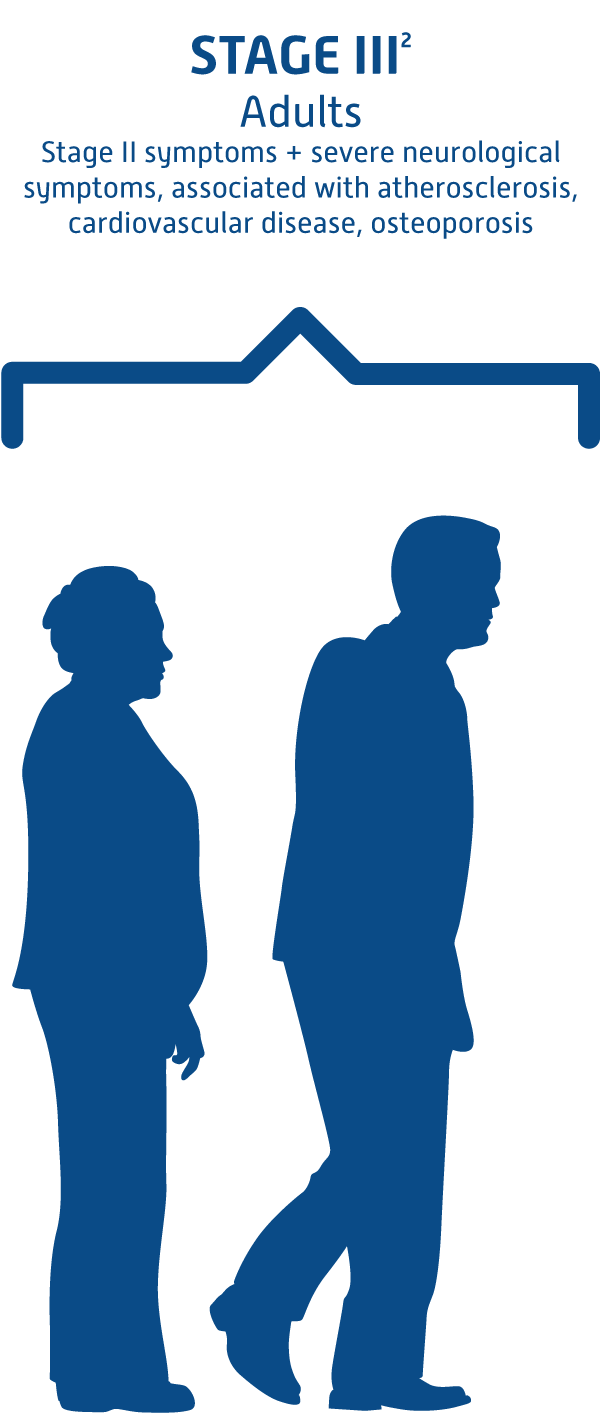
It is important to understand that the signs and symptoms of CTX vary from patient to patient, and neurological symptoms can worsen over time.
Hallmark Manifestations
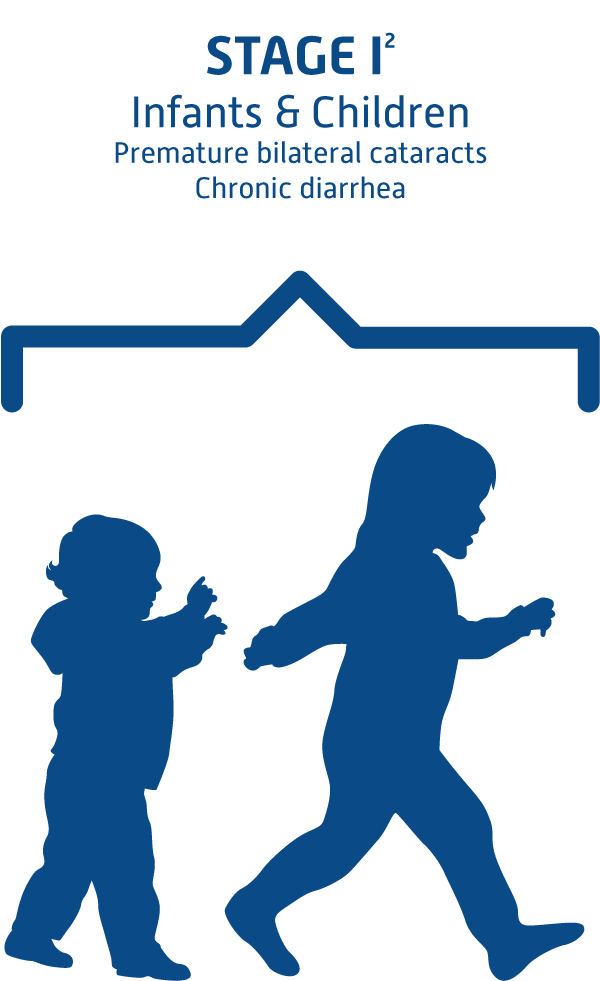
- Chronic diarrhea beginning during infancy is a hallmark symptom.
- Cataracts in both eyes commonly appear in children and adolescents, although they may not develop at the same time and may occur later in life.
- Xanthomas, or fatty, yellow deposits in the tendons and other organs, may develop in adolescents and young adults, and most commonly on the knees, Achilles tendons, and elbows.
- Severe neurological signs of the disease (seizures, dementia, movement disorders) usually become apparent in young adulthood. However, in some cases, neurological symptoms such as decreased muscle coordination, abnormal reflexes, and intellectual decline can occur as early as adolescence, and cognitive impairment, developmental delays, and epilepsy may appear during childhood.1,2